NEW YORK–(BUSINESS WIRE)–May 4, 2020–
This week, results from Sermo’s COVID-19 Real Time Barometer with over 5,900 physicians explored whether COVID-19 was a new type of disease, the controversial use of ventilators, as well as the new protocols that could change the way physicians treat COVID-19. In total, Sermo’s Barometer study includes over 27,000 survey interviews in 31 countries, including the United States, Canada, United Kingdom, France, Brazil, Russia, China, Japan and Australia. All data published to date and study methodology can be found .
This press release features multimedia. View the full release here:
Visit sermo.com for full survey results (Graphic: Business Wire)
Knowledge of COVID-19 and the optimal treatment approach is evolving, and some voices on the front lines have relayed they are charting unfamiliar territory and broadcasting concerns over treatment approaches, particularly the use of ventilators. The statistics around the much sought after breathing device are sobering. In NY, up to 88% of those placed on ventilators died (1). “Panic buying of ventilators” and competition among states to procure ventilators was intense at the onset of the COVID-19 outbreak.
Dr. Cameron Kyle-Sidell, a New York-based ER and critical care physician widely broadcast a compelling message on YouTube, “we are treating the wrong disease.” (2) We wanted to further probe his theory and formulated structured questions which were later taken to thousands of international physicians on the front lines.
“Nine days ago I opened an intensive care unit to care for the sickest COVID patients. In these 9 days I’ve seen things I’ve never seen before. I presumed I was opening an ICU to treat patients with a virus causing pneumonia that started out mild — and progressed in severity, ultimately ending in acute respiratory distress syndrome or ARDS. ARDS is the disease that every hospital is preparing to treat. And for which many patients might be put on a ventilator. And yet, everything I’ve seen in the last 9 days just doesn’t make sense…I believe we are treating the wrong disease. COVID-19 lung disease…is not a pneumonia and should not be treated as one. Rather, it appears as if it’s some kind of viral-induced disease most resembling high altitude sickness…as if (patients) are on a plane at 30,000 feet and the cabin pressure is slowly being let out. These patients are being starved of oxygen…they eventually get blue in the face, and while they look like patients on the brink of death, they do not look like patients dying of pneumonia…they look more like (they were) dropped off at the top of Mount Everest without time to acclimate.
“I don’t know the final answer to this disease but I’m quite sure that a ventilator is not it. That is not to say that we don’t need ventilators, they are the only way at this time that we are able to give a little more oxygen to patients who need it. But when we treat ARDS, we typically use ventilators to treat respiratory failure, the ventilator does the work that the patients’ muscles can no longer do because they are too tired. These patients’ muscles work fine. I fear that if we are using a false paradigm to treat a new disease that the method that we program the ventilator, one based on a notion of respiratory failure as opposed to oxygen failure, (and there are a great many number of methods we can use with the ventilator), a method being widely adopted in every hospital in the country which aims to increase pressure on the lungs in order to open them up, is actually doing more harm than good…the pressure we are providing to lungs, may not be able to take it, and that the ARDS that we are seeing, may be nothing more than lung injury caused by the ventilator. Now, I don’t know the final answer to this disease. I do sense that we will have to use ventilators, but in a safer way. That safer method challenges long-held dogmatic beliefs within the medical community and among lung specialists which will not be easy to overcome.”
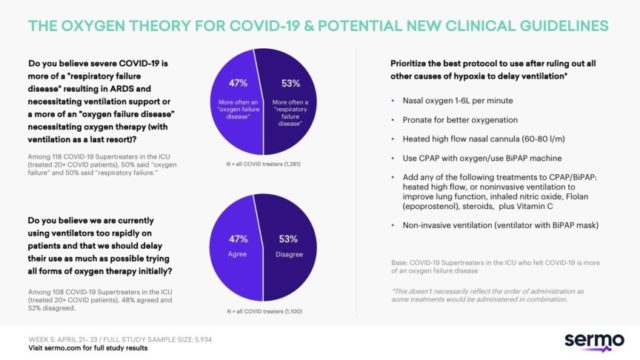
In our analysis of results from this past week, we focused on the responses from all physicians treating COVID-19 as well as “COVID-19 Supertreaters in the ICU” (physicians who have treated over 20 COVID-19 patients) and presumably would have the most educated opinions on the matter.
“My theory on the split in opinions is that in the beginning of this outbreak, patients were coming in and deteriorating so rapidly that healthcare providers were rushing to help patients breathe in whatever way they could,” said Dr. Mark Rumbak, Sermo physician and pulmonologist. “We are starting to rethink this.”
The two are results related; 63% of physicians who believed COVID-19 to be more of an oxygen failure disease also believed we are using ventilators too rapidly.
“What’s highly significant here is that there should be almost unanimous opinion on these topics as we have guidelines for Acute Respiratory Distress Syndrome (ARDS) treatment. What we are seeing is ARDS caused by pneumonia (this was found histologically), it just responds differently. Usually ARDS responds to higher PEEP and low FiO2. This COVID-19 ARDS seems to do worse with higher PEEP levels and better with higher oxygen levels. Why does this COVID-19 ARDS respond differently from the regular ARDS? It seems with COVID-19 patients there is multi-organ failure and, when the heart is damaged, higher PEEP will cause decreased cardiac function and hypoxia. There is an increase in clotting and pulmonary embolus and clots in lungs and heart may cause shunting (when blood bypasses the lungs and hypoxia is increased). Therefore, the treatment of ARDS in these patients is low tidal volumes, high oxygen and lower PEEP.”
Anonymous pulmonologist Sermo member, “It could be a mix of both, perhaps we need to treat that oxygen failure much earlier, more rapidly and with diverse oxygen therapies.”
Only 17% of physicians felt that the majority of patients (60% – 100%) respond to ARDS strategies.
?
We explored other treatments and drugs that could be used to improve oxygenation/ delay intubation. Again, we report on COVID-19 Supertreaters in the ICU.
81%
64%
29%
8%
19%
19%
10%
2%
There are alternative oxygen therapies that aren’t standard protocol for COVID-19 patients but are starting to see some use. The ECMO machine (extracorporeal membrane oxygenation), also known as extracorporeal life support, is an extracorporeal technique of providing prolonged cardiac and respiratory support to persons whose heart and lungs are unable to provide an adequate amount of gas exchange or perfusion to sustain life. Hyperbaric oxygen therapy involves breathing pure oxygen in a pressurized room or tube and is a well-established treatment for decompression sickness from scuba diving, serious infections, bubbles of air in the blood vessels, and non-healing wounds resulting from diabetes or radiation.
“ECMO is an alternative and is used when P/F ratio drops below 80. Although there are less ECMO machines than ventilators they will decrease the amount of ventilators used. Some patients can be extubated while on ECMO and the ventilators used on other patients. ECMO may save lives. ECMO machines are the same machines used in cardiac surgery. As most routine cardiac surgical cases are not being performed due to COVID-19, they can be used in the ICU. Perhaps we could also use hyperbaric chambers although there are not too many of these. We could try to increase their supply. Some have suggested using the many idle airplanes we have and pressurizing the cabins to produce ‘hyperbaric’ oxygen. Many patients can be treated in one plane safely,” said Dr. Rumbak.
28% (n=396 COVID-19 treaters with opinion on Hyperbaric oxygen)
44% (n=467 COVID-19 treaters with opinion on ECMO)
31% (n=45 COVID-19 Supertreaters in the ICU with opinion on Hyperbaric oxygen)
39% (n=54 COVID-19 Supertreaters in the ICU with opinion on ECMO)
We asked the physicians who felt COVID-19 is more of an oxygen failure issue to build a protocol where they ordered eight different oxygen strategies presented in order of priority to delay intubation. We asked physicians to place these strategies in order of what would be the best protocol to use after ruling out all other causes of hypoxia (heart failure, blood clot, cirrhosis, collapsed lung, shunts heart damage).
Overall this was the order of top priority for the following strategies; however, this doesn’t necessarily reflect the order of administration as some treatments would be administered in combination.
Sermo is the largest healthcare data collection company and social platform for physicians, reaching 1,3MM HCPs across 150 countries. The platform enables doctors to anonymously talk real-world medicine, review treatment options via our proprietary Drug Ratings platform, collectively solve patient cases, and participate in medical market research. For more information, visit .
View source version on businesswire.com:
CONTACT: Brooke Matthews
805-252-5483
KEYWORD: NEW YORK UNITED STATES NORTH AMERICA
INDUSTRY KEYWORD: WOMEN MANAGED CARE MEN GENERAL HEALTH HEALTH MEDICAL DEVICES INFECTIOUS DISEASES CONSUMER
SOURCE: Sermo
Copyright Business Wire 2020.
PUB: 05/04/2020 09:00 AM/DISC: 05/04/2020 09:01 AM
COMMENTS
Please let us know if you're having issues with commenting.